Abstract
Cutaneous T-cell lymphomas (CTCL) have a wide spectrum of clinical, histological, immunophenotypic features and genetic alterations which make their diagnosis challenging. Due to the rarity and poor characterization of Primary cutaneous CD8-positive aggressive epidermotropic T-cell lymphoma ((PCAECyTCL), it remains a provisional entity in WHO classification (2018) (1).
The constant immunohistochemical finding in PCEACyTCL is CD8 +/ CD4 - expression that is non-specific. So, it needs a consensus on the correlation of clinical & lab for accurate diagnosis (2).In addition to the aggressive presentation of the disease and the associated burden of infection make treatment decisions very challenging.
Herein, we are presenting our experience in treating an aggressive case of PCEACyTCL, and how we dealt with the disease and its complications.
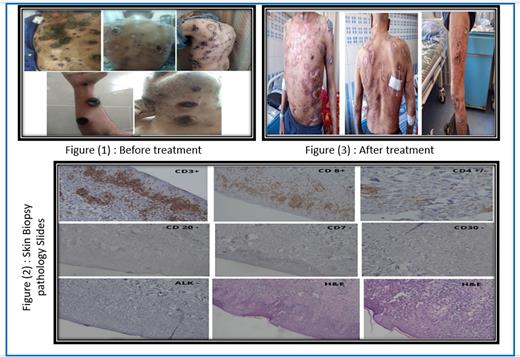
a 58-year-old male, with a history of Psoriasis, started with him 30 years and he was on topical treatment for it. Referred to us after 3 months journey in the Dermatological department with rapidly progressive maculopapular lesions & tumors, showing central ulcerations, necrosis, and complicated by purulent bacterial infection involving his face, scalp, neck, all 4 limbs, whole trunk, perineum with the oral cavity and oropharynx. There was also generalized lymphadenopathy (Figure 1). His lab results were within the normal range with no evidence of any abnormal infiltration by lymphocytes in peripheral blood and Bone marrow examination. Punch skin biopsy showed that the dermis was the seat of dense localized upper & mid dermal wedge-shaped angiocentric & perivascular inflammatory cell infiltrate composed mainly of activated lymphocytes mixed with histiocytes, plasma cells & neutrophils with atypical, transformed lymphocytes. The infiltrate is encroaching upon the epidermis with degeneration of the basal cell layer & epidermotropism. The Immunohistochemistry revealed diffuse positivity of CD3, weak positivity of CD4, and strong positivity of CD8 with negativity for CD7, CD20, CD30, and ALK in the atypical, transformed T-lymphocytes (Figure 2). The patient was diagnosed to have pcAECyTCL. The staging was done using Contrast CT of the chest, abdomen, and pelvis and showed generalized lymphadenopathy with pulmonary nodules, so he was staged (IVB).
After mild improvement of the patient's general condition by anti-biotics, painkillers, and supportive treatment, he started CHOP/Etoposide (doxorubicin 50 mg/m2, cyclophosphamide 750 mg/m2, and vincristine 1.4 mg/m2 by intravenous infusion on day 1, etoposide 100 mg/m2 intravenously days 1-3) to be repeated/3 weeks, with G-CSF as our patient showed aggressive myelosuppression after cycles.
There was a very promising improvement in his skin lesions (Figure 3), oral ulcers, and general condition. After 3 cycles of chemotherapy, a PET scan showed: Non metabolically active lymphadenopathy. Metabolically active diffuse skin lesions forming irregular skin thickening over the trunk & limbs (SUV max 5). So, he continued further 3 cycles with preparation for an ASCT.
Unfortunately, before stem cell transplantation, the skin lesions progressed again with the same aggression. So, he was given 1 cycle of GEMOX (Gemcitabine1 gm/m2 and Oxaliplatin 100 mg/m2 to be repeated/14 days) then he got COVID-19 infection and is still under treatment for it.
In our patient, psoriasis can be considered a susceptible predisposing factor for pcAECyTCL according to the proposed theory by Cai, Fleming and Yan, and others (3,4).
One of the obvious problems of pcAECyTCL is the exhibition of T-helper-1 cytokine profile, this makes many treatment options inappropriate as Interferons (5). Theoretically, multi-agent chemotherapies appear to be better options, but they carry the risk of toxicity and myelosuppression, and their response is unsatisfactory till now. There are emerging novel therapies but still not applied to this type of lymphoma due to its rarity (6, 7, 8). Bastidas et al. was suggesting that Ruxolitinib may play a future role in its treatment, but this is still in need of future research (9).
The CHOP/etoposide protocol was promising in our patient, but it didn't give a durable response. The plan after improvement from COVID-19 infection is to give a targeted therapy as Brentuximab if available or an aggressive protocol as Hyper-CVAD followed by ASCT hoping for CR, longer OS, and better quality of life.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal